Table of Contents
Introduction
We begin by acknowledging that the liver plays a vital role in maintaining our overall health. It is responsible for filtering toxins, producing essential proteins, metabolizing nutrients, and aiding in digestion. Therefore, any Liver failure, disruption, or insufficiency in its functioning can have severe consequences for our well-being.
Liver failure is a condition where the liver loses its ability to perform these crucial functions adequately. It can occur suddenly (acute liver failure) or develop gradually over time (chronic liver failure). Understanding the clinical manifestations of liver failure is essential for early detection and timely intervention.
One of the primary signs of liver failure is jaundice, characterized by yellowing of the skin and eyes due to a buildup of bilirubin. Fatigue, weakness, and unexplained weight loss are also common symptoms. As liver function declines, individuals may experience abdominal pain, swelling in the legs and abdomen, and easy bruising or bleeding.
Clinical Manifestations of Liver Failure
Early recognition of these signs is crucial because liver failure can progress rapidly and lead to life-threatening complications if left untreated. Abdominal swelling, also known as ascites, occurs due to fluid accumulation in the abdominal cavity.
This happens when the liver fails to produce enough albumin, a protein responsible for maintaining fluid balance in the body. Ascites can cause discomfort, difficulty breathing, and increased pressure on other organs.
Jaundice is another common symptom of liver failure. It manifests as yellowing of the skin and eyes due to a buildup of bilirubin, a yellow pigment produced during the breakdown of red blood cells.
When the liver is unable to process bilirubin effectively, it accumulates in the bloodstream and causes this characteristic discoloration. Jaundice may also be accompanied by dark urine and pale stools.Fatigue is a prevalent symptom experienced by individuals with liver insufficiency. The liver plays a vital role in metabolizing nutrients and producing energy for the body.
Abdominal Swelling: A Telltale Sign of Liver Failure
In cases of liver failure, the liver’s ability to function properly is compromised, leading to various symptoms. Abdominal swelling, or ascites, occurs as a result of the liver’s inability to produce enough albumin, a protein responsible for maintaining fluid balance in the body. Without sufficient albumin production, fluid begins to accumulate in the abdominal cavity.
The accumulation of fluid in the abdomen can cause discomfort and a feeling of fullness. As ascites progress, it may lead to increased pressure on surrounding organs such as the stomach and intestines. This pressure can cause bloating and make it difficult for individuals to eat or drink normally.
Furthermore, ascites can also exert pressure on blood vessels within the abdomen, leading to impaired circulation. This can result in swollen legs and ankles due to fluid retention and poor blood flow.
Aside from abdominal swelling, other signs of liver failure may include jaundice (yellowing of the skin and eyes), fatigue, weakness, loss of appetite, and nausea.
Jaundice: Understanding the Yellow Hue
Jaundice occurs when there is an excess of bilirubin in the bloodstream. Bilirubin is a yellow pigment that is produced when red blood cells break down. Normally, the liver processes and eliminates bilirubin from the body. However, when the liver is not functioning properly, it fails to efficiently remove bilirubin, leading to its accumulation in the body.
Liver dysfunction can occur due to various reasons such as hepatitis, alcohol abuse, certain medications, or liver diseases like cirrhosis. When the liver is unable to process bilirubin effectively, it builds up in the bloodstream and eventually gets deposited in body tissues, causing a yellowish discoloration of the skin and eyes known as jaundice.
Beyond its visible symptoms, jaundice serves as an important indicator of overall health. The liver plays a crucial role in numerous bodily functions including detoxification, metabolism of nutrients, production of bile for digestion, and synthesis of essential proteins.
Fatigue and Weakness: The Unseen Struggle of Liver Failure
When the liver fails to function properly, it affects the body’s ability to process and store nutrients, leading to a decrease in energy levels. The liver plays a crucial role in metabolizing carbohydrates, proteins, and fats, which are essential for providing energy to the body. Therefore, any disruption in its normal functioning can result in persistent fatigue and weakness.
Initially, these symptoms may be mild and easily overlooked. People may attribute their tiredness to stress or lack of sleep. However, as liver failure progresses, the impact on daily life becomes more evident. Simple tasks that were once effortless now require significant effort and can leave individuals feeling exhausted.
Understanding the correlation between liver health and energy levels is vital for comprehensive well-being. By recognizing the early signs of liver dysfunction, such as fatigue and weakness, individuals can seek medical attention promptly. Early intervention can help prevent further damage to the liver and improve the overall quality of life.
Causes of Liver Failure
Understanding the root causes of liver failure is crucial for developing effective strategies to address this complex condition. Viral infections, such as hepatitis B and C, are among the leading causes of liver insufficiency worldwide. These infections can cause chronic inflammation and damage to the liver cells over time, eventually leading to liver failure if left untreated.
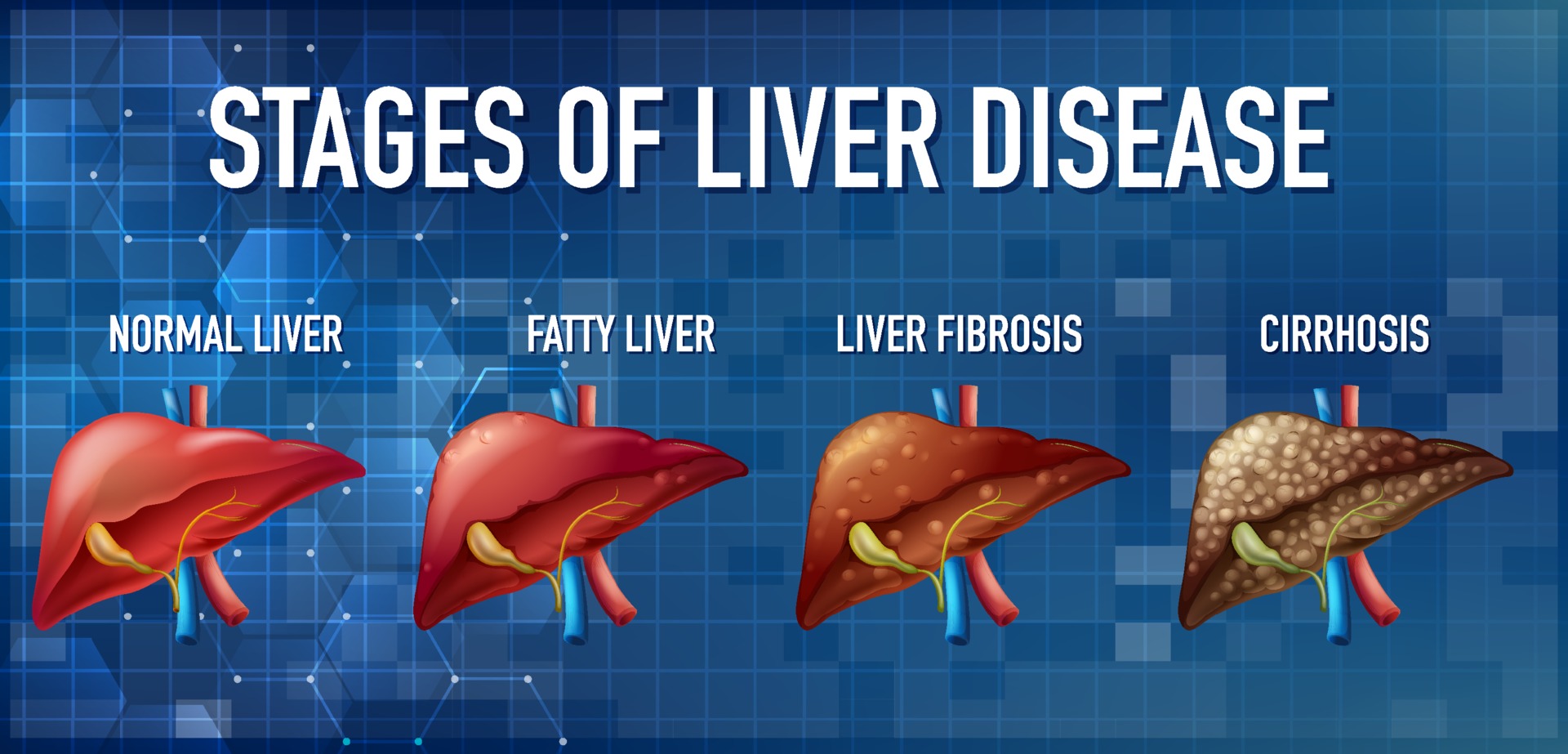
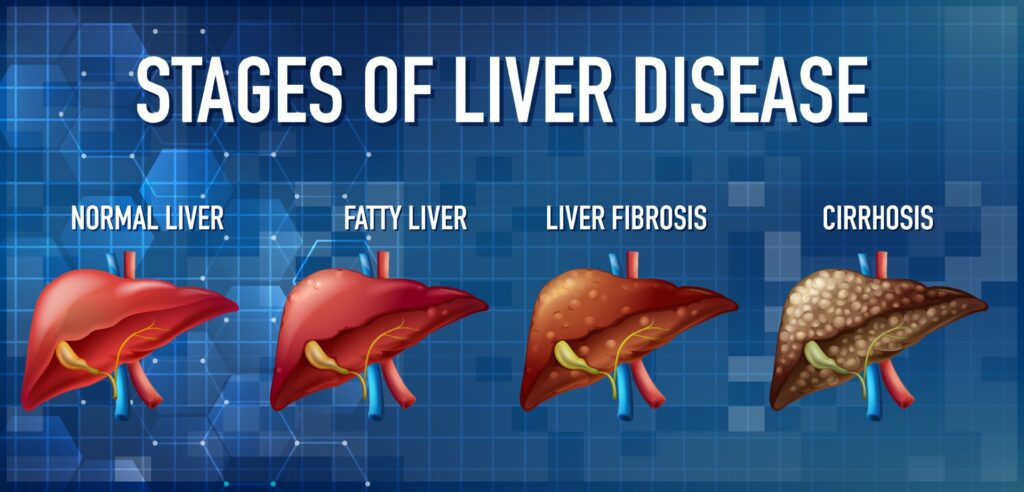
Another significant factor contributing to liver failure is excessive alcohol consumption. Alcohol abuse can lead to alcoholic liver disease, which encompasses a spectrum of conditions ranging from fatty liver to alcoholic hepatitis and cirrhosis. Prolonged alcohol abuse puts immense stress on the liver, impairing its ability to function properly and potentially resulting in irreversible damage.
Non-alcoholic fatty liver disease (NAFLD) is also emerging as a prevalent cause of liver failure. This condition is closely associated with obesity, insulin resistance, and metabolic syndrome. NAFLD occurs when excess fat accumulates in the liver cells, causing inflammation and scarring that can progress to more severe conditions.
Viral Infections: Unraveling the Hepatitis Connection
Viral hepatitis, specifically Hepatitis B and C, is a major concern due to its potential to cause liver failure. To effectively combat this threat, it is essential to delve into the modes of transmission, preventive measures, and available treatments.
Understanding the modes of transmission is crucial in preventing the spread of viral hepatitis. Hepatitis B can be transmitted through contact with infected blood or bodily fluids, such as during unprotected sexual intercourse, sharing needles or syringes, or from an infected mother to her newborn during childbirth. On the other hand, Hepatitis C is primarily transmitted through exposure to infected blood, often resulting from sharing needles or receiving contaminated medical procedures.
To safeguard liver health and prevent the transmission of viral hepatitis, various preventive measures should be adopted. Vaccination against Hepatitis B is highly effective in preventing infection and subsequent liver damage. It is recommended for all infants at birth and for individuals at higher risk due to their occupation (e.g., healthcare workers), lifestyle choices (e.g., multiple sexual partners)
Alcohol Consumption: Balancing Act for Liver Health
Excessive alcohol consumption is a well-established contributor to liver dysfunction. The liver plays a crucial role in metabolizing alcohol, but when the intake exceeds its capacity, it can lead to serious health consequences. However, it is important to note that responsible drinking habits can help maintain a delicate balance between alcohol intake and liver health.
Responsible drinking involves understanding and adhering to recommended guidelines for alcohol consumption. These guidelines vary across countries but generally suggest moderate drinking for adults, which means up to one drink per day for women and up to two drinks per day for men. It is essential to be aware of these limits and not exceed them regularly.
Furthermore, spacing out the consumption of alcoholic beverages over time allows the liver to process the alcohol more efficiently. This gives the organ enough time to metabolize the alcohol without being overwhelmed by its toxic effects. Drinking slowly and alternating alcoholic beverages with non-alcoholic ones can also help reduce overall alcohol intake.
Non-Alcoholic Fatty Liver Disease (NAFLD): The Silent Threat
NAFLD, or non-alcoholic fatty liver disease, has become a significant concern in recent years due to its close association with obesity and metabolic syndrome. As the prevalence of these conditions continues to rise globally, so does the incidence of NAFLD, making it an emerging cause of liver failure.
Understanding the intricacies of NAFLD is crucial in order to develop effective preventative measures and lifestyle modifications that can help mitigate its impact. This condition occurs when excess fat accumulates in the liver cells of individuals who consume little to no alcohol. It is often characterized by inflammation and can progress to more severe forms such as non-alcoholic steatohepatitis (NASH), fibrosis, cirrhosis, and even hepatocellular carcinoma.
Obesity and metabolic syndrome play a significant role in the development and progression of NAFLD. Excess body weight, particularly abdominal obesity, increases insulin resistance and promotes fat accumulation in the liver.
Consequences of Untreated Liver Failure
One of the most critical consequences of untreated liver failure is the development of hepatic encephalopathy. This condition occurs when the liver fails to remove toxins, such as ammonia, from the bloodstream.
As a result, these toxins accumulate in the brain, leading to cognitive impairment, confusion, personality changes, and even coma in severe cases. Hepatic encephalopathy not only affects the individual’s mental state but also impacts their overall quality of life.
Furthermore, untreated liver failure can lead to complications in the cardiovascular system. The liver plays a crucial role in regulating blood flow throughout the body by producing proteins that help maintain proper blood pressure.
When liver function deteriorates, these proteins are not adequately produced, resulting in increased pressure within the blood vessels. This condition is known as portal hypertension and can lead to life-threatening complications like variceal bleeding or ascites (abdominal fluid accumulation).Another organ system affected by untreated liver failure is the digestive system.
Hepatic Encephalopathy: Navigating Cognitive Impacts
Hepatic encephalopathy is a condition that occurs when the liver fails to remove toxins from the blood, leading to a buildup of harmful substances in the body. As these toxins accumulate, they can cross the blood-brain barrier and affect brain function, resulting in cognitive impairment.
One of the first signs of hepatic encephalopathy is often subtle changes in behavior and personality. Individuals may experience confusion, forgetfulness, difficulty concentrating, and mood swings. As the condition progresses, more severe symptoms such as disorientation, slurred speech, tremors, and even coma can occur.
Recognizing these signs is crucial for early intervention and treatment. If left untreated, hepatic encephalopathy can significantly impact an individual’s mental well-being and overall quality of life.
Therefore, it is essential for healthcare professionals to be vigilant when monitoring patients with liver insufficiency for any cognitive changes.Treatment options for hepatic encephalopathy aim to reduce toxin levels in the body and manage symptoms.
Ascending Complications: Beyond the Liver
Liver failure is a critical condition that can have far-reaching consequences beyond just the liver itself. When the liver fails to function properly, it not only impairs its own ability to detoxify harmful substances and produce essential proteins but also disrupts the delicate balance of other organ systems.
One of the major complications that arise from liver failure is kidney dysfunction. The kidneys play a crucial role in filtering waste products and maintaining fluid and electrolyte balance in the body.
However, when the liver fails, it can lead to a buildup of toxins and metabolic byproducts in the bloodstream, which puts an excessive burden on the kidneys. This overload can result in impaired kidney function, leading to fluid retention, electrolyte imbalances, and even acute kidney injury.
Liver failure has profound effects on the cardiovascular system. The liver plays a key role in regulating blood flow by producing clotting factors and synthesizing proteins that maintain blood volume and pressure.

Conclusion
Furthermore, this guide emphasizes the importance of early detection and diagnosis of liver failure. By recognizing the warning signs and seeking medical attention promptly, individuals can increase their chances of receiving timely interventions and treatments that may slow down or even reverse the progression of liver damage.
Moreover, this comprehensive resource sheds light on the various causes of liver failure, including alcohol abuse, viral infections (such as hepatitis B and C), obesity, autoimmune diseases, and certain medications.
By understanding these risk factors, individuals can make informed decisions about their lifestyle choices and take the necessary precautions to protect their liver health.
Additionally, this guide highlights the potential consequences of untreated liver failure. From jaundice and ascites to hepatic encephalopathy and hepatocellular carcinoma, the complications associated with advanced liver disease can be severe and life-threatening.
By educating individuals about these potential outcomes, we hope to motivate them to prioritize regular check-ups and adopt healthy habits that support liver function.
Frequently Asked Questions
Q1. What are the common causes of liver failure?
Liver failure can be caused by various factors, including chronic alcohol abuse, viral hepatitis (such as hepatitis B and C), fatty liver disease, autoimmune conditions (such as autoimmune hepatitis), certain medications and toxins, genetic disorders, and liver cancer. Identifying and addressing the underlying cause is crucial for preventing or managing liver failure.
Q2. What are the early signs and symptoms of liver failure?
Early signs of liver failure may include fatigue, weakness, loss of appetite, nausea, vomiting, abdominal pain or swelling, jaundice (yellowing of the skin and eyes), dark urine, pale stools, itching, easy bruising or bleeding, and mental confusion.
It’s essential to seek medical attention if experiencing any of these symptoms, as early detection and treatment can improve outcomes.
Q3. How is liver failure diagnosed?
Diagnosis of liver failure typically involves a combination of medical history evaluation, physical examination, blood tests to assess liver function and detect markers of liver damage, imaging studies (such as ultrasound, CT scan, or MRI) to evaluate the liver’s structure, and sometimes a liver biopsy to assess the extent of liver damage and determine the underlying cause.
Q4. What are the treatment options for liver failure?
Treatment for liver failure depends on the underlying cause and severity of the condition. In some cases, lifestyle modifications such as abstaining from alcohol, maintaining a healthy diet, and managing underlying medical conditions may be sufficient.
For more advanced cases, treatment options may include medications to manage symptoms and complications, liver transplant surgery for severe liver damage, and supportive care to alleviate discomfort and improve quality of life.
Q5. Can liver failure be prevented?
While not all causes of liver failure are preventable, adopting a healthy lifestyle can reduce the risk of liver damage and disease.
This includes avoiding excessive alcohol consumption, maintaining a healthy weight through diet and exercise, practicing safe sex and avoiding sharing needles to prevent viral hepatitis, getting vaccinated against hepatitis A and B, avoiding exposure to toxins and chemicals, and following prescribed medication regimens as directed by healthcare providers.
Regular medical check-ups and screenings can also help detect liver problems early and facilitate prompt intervention if needed.